| Click here to see a web copy of this news release | |
|
FOR IMMEDIATE RELEASE Why Vitamin D Fails to Rise in Many People: New Evidence - and How Orthomolecular Medicine Solves Itby Richard Z. Cheng, M.D., Ph.D. IntroductionMillions of people take Vitamin D or spend time in the sun, yet their blood Vitamin D levels barely improve. Others supplement modestly and reach optimal levels quickly. This long-standing clinical puzzle is finally gaining scientific clarity. A major 2025 Nature Communications study [1] identified over 160 genetic variants that affect Vitamin D status. Combined with research on micronutrient cofactors, metabolic health, and inflammation, the evidence points to a key conclusion: Vitamin D deficiency is rarely a "single-nutrient problem." It is a systems-biology problem. Orthomolecular Medicine offers a complete solution. 1. Genetics Explains Why People Respond So DifferentlyShraim et al. (Nature Communications, 2025) [1] found 162 variants affecting:
Implications:
Genetics sets the baseline - but genes are not the full story. See Figure 1 for visualization of the wide genetic variability in Vitamin D response. 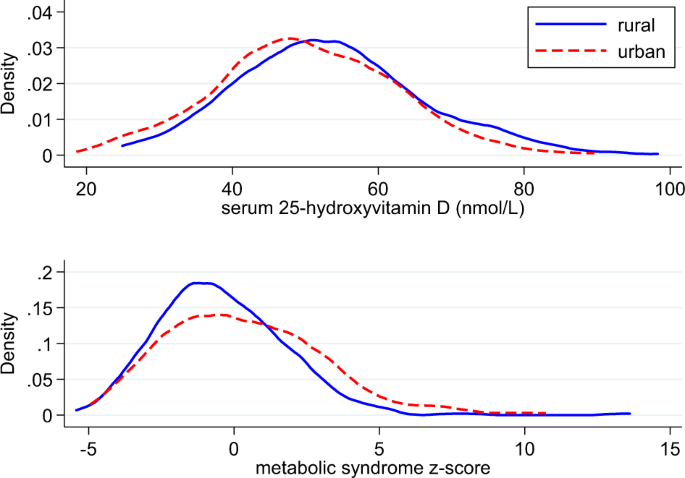
Figure 1. Genetic Diversity in Vitamin D Response This figure illustrates why two people taking the same supplement dose may show very different 25(OH)D levels-including one rising rapidly and the other barely changing. The 162 identified gene variants affect Vitamin D production in the skin, activation in liver/kidney, transport proteins, and receptor sensitivity (data from [1]). 2. "Vitamin D Resistance": The Missing DiagnosisIn my 2024 OMNS review, I proposed that many individuals exhibit acquired Vitamin D resistance [2]: Vitamin D is present, but cannot activate or function properly. Drivers include:
This explains why many people experience: "Vitamin D doesn't work for me." The problem is not the Vitamin D - it is the internal metabolic environment. 3. Vitamin D Needs Its Team: The Essential CofactorsVitamin D metabolism and receptor activity depend on:
Without these cofactors, functional Vitamin D deficiency develops - even with "normal" blood levels. General Cofactor Ranges (Individual needs vary, but the following ranges apply to most adults.)
This is a core principle of Orthomolecular Medicine. 4. How Much Vitamin D Is Safe? The Evidence Is ClearThe overall benefit curve of serum 25(OH)D - how health outcomes improve up to the 60-80 ng/mL range - is shown in Figure 2. 
Figure 2. Vitamin D Benefit Curve This chart shows the rapid rise in health benefits (immunity, metabolic function, bone health, mortality reduction) as serum 25(OH)D increases from 10 → 40 ng/mL, with a plateau around 60-80 ng/mL-the optimal physiological range (data from [3-12] ). Optimal Range
Safety Profile
Vitamin D remains one of the safest nutrients in modern medicine. See Figure 3 for the Vitamin D toxicity curve and documented hypercalcemia thresholds. 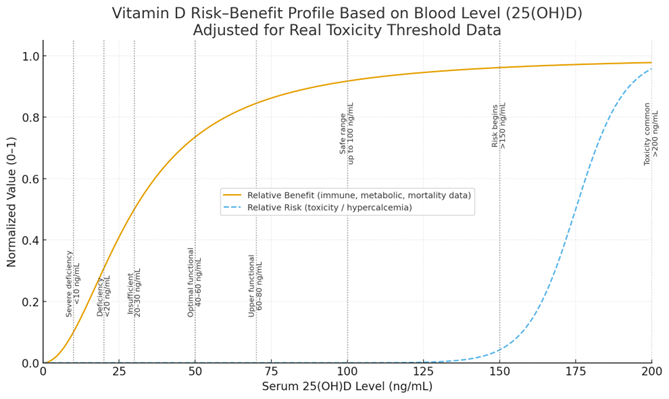
Figure 3. Vitamin D Safety Curve This figure shows that real toxicity is extremely rare below 150 ng/mL, and documented toxicity occurs only when blood levels exceed 200 ng/mtheL, typically from accidental massive overdosing (data from [3-12]. 5. A Real-World Case: When Higher Doses Are NecessaryCase 1: Husband-Wife GrassrootsHealth CohortA woman maintained 40-60 ng/mL on 2,000 IU/day.
Lesson: metabolic inflammation and genetics radically alter dose requirements. Some individuals - particularly those with inflammation, obesity, or genetic variations - simply require higher doses. Case 2: High-Dose IndividualA man in his 60s took 30,000 IU/day for 30 days. Follow-up:
This is within the low-risk / high-benefit zone repeatedly documented in large cohorts. Case 3: Severe Hypercalcemia and Renal Impairment Induced by Prolonged High-Dose Vitamin D3 SupplementationA 23-year-old previously healthy male had been taking high-dose vitamin D3 (50,000 IU daily) for several consecutive months, along with a multivitamin supplement containing calcium. He subsequently developed biochemical evidence of severe vitamin D intoxication. He was then referred to me.
This case illustrates the potential dangers of unsupervised high-dose vitamin D supplementation, especially when combined with exogenous calcium, leading to life-threatening hypercalcemia and renal impairment. 6. Lifestyle & Endocrine Factors Are IntegralVitamin D status is influenced by:
These factors align with the Orthomolecular view that nutrients do not work alone - they function within the body's entire biochemical network. 7. Practical Orthomolecular Recommendations1. Test Beyond 25(OH)D
2. Individualize the dose Typical effective ranges:
3. Always include cofactors
4. Improve lifestyle factors
5. Recheck levels every 3-6 months ConclusionVitamin D is not simply "take a pill and your level rises." It reflects a complex integration of: Genes × Sunlight × Micronutrients × Metabolism × Inflammation × Endocrine Health = Necessity of a Personalized Dose Orthomolecular Medicine restores the entire biochemical terrain - enabling Vitamin D to function as intended. 8. This Is One More Example of the Root-Cause Model of Chronic DiseaseVitamin D resistance is not an isolated phenomenon. It exemplifies a deeper truth: Chronic diseases arise from disruptions across multiple root drivers - genetic, metabolic, inflammatory, toxic, nutritional, and endocrine. As I detailed in: Cheng, R. Z. From Mutation to Metabolism: Root Cause Analysis of Cancer's Initiating Drivers [13]. Health and disease are determined not by a single molecule (like vitamin C or D) or a single mechanism (like mitochondrial dysfunction or gut dysbiosis), but by the interconnected matrix of:
Vitamin D resistance is simply one more illustration of this unifying principle: To restore health, we must identify and correct as many root drivers as possible - not chase downstream symptoms or the mechanism between root drivers and clinical diseases. Orthomolecular Medicine is the framework that recognizes and addresses these root drivers systematically. About the AuthorRichard Z. Cheng, M.D., Ph.D. is Editor-in-Chief of the Orthomolecular Medicine News Service. He is a U.S.-based, NIH-trained, board-certified physician specializing in integrative oncology, orthomolecular medicine, and metabolic/functional medicine, with clinical practices in both the United States and China. Dr. Cheng is a Hall of Fame inductee of the International Society for Orthomolecular Medicine and a Fellow of the American Academy of Anti-Aging and Regenerative Medicine (A4M). He has been active in advancing nutrition-based, root-cause approaches to chronic disease, co-founding the China Low Carb Medicine Alliance and serving as an expert reviewer for the South Carolina Board of Medical Examiners. He is the author of the forthcoming book 21st Century Medicine: Integrative Orthomolecular Medicine for Chronic Disease Reversal and Longevity, which summarizes insights from five decades of clinical practice and research. More of Dr. Cheng's writings are available at: https://substack.com/@rzchengmd References1. Shraim, R.; Timofeeva, M.; Wyse, C.; Geffen, J. van; Weele, M. van; Romero-Ortuno, R.; Lopez, L.M.; Kleber, M.E.; Pilz, S.; März, W.; Fletcher, B.S.; Wilson, J.F.; Theodoratou, E.; Dunlop, M.G.; McManus, R.; Zgaga, L. Genome-Wide Gene-Environment Interaction Study Uncovers 162 Vitamin D Status Variants Using a Precise Ambient UVB Measure. Nat Commun 2025, 16, (1), 10774. DOI: 10.1038/s41467-025-65820-x. 2. Cheng, R.Z. Understanding and Addressing Vitamin D Resistance: A Comprehensive Approach Integrating Genetic, Environmental, and Nutritional Factors. Orthomolecular Medicine News Service 2024, 20, (13).; Available online: https://orthomolecular.org/resources/omns/v20n13.shtml. 3. Manson, J.E.; Cook, N.R.; Lee, I.-M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Gordon, D.; Copeland, T.; D'Agostino, D.; Friedenberg, G.; Ridge, C.; Bubes, V.; Giovannucci, E.L.; Willett, W.C.; Buring, J.E.; VITAL Research Group Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med 2019, 380, (1), 33-44. DOI: 10.1056/NEJMoa1809944. 4. Garland, C.F.; Kim, J.J.; Mohr, S.B.; Gorham, E.D.; Grant, W.B.; Giovannucci, E.L.; Baggerly, L.; Hofflich, H.; Ramsdell, J.W.; Zeng, K.; Heaney, R.P. Meta-Analysis of All-Cause Mortality According to Serum 25-Hydroxyvitamin D. Am J Public Health 2014, 104, (8), e43-50. DOI: 10.2105/AJPH.2014.302034. 5. McDonnell, S.L.; Baggerly, C.; French, C.B.; Baggerly, L.L.; Garland, C.F.; Gorham, E.D.; Lappe, J.M.; Heaney, R.P. Serum 25-Hydroxyvitamin D Concentrations ≥40 Ng/Ml Are Associated with >65% Lower Cancer Risk: Pooled Analysis of Randomized Trial and Prospective Cohort Study. PLoS One 2016, 11, (4), e0152441. DOI: 10.1371/journal.pone.0152441. 6. Vieth, R. Vitamin D Toxicity, Policy, and Science. J Bone Miner Res 2007, 22 Suppl 2, V64-68. DOI: 10.1359/jbmr.07s221. 7. Vieth, R. Vitamin D Supplementation, 25-Hydroxyvitamin D Concentrations, and Safety. Am J Clin Nutr 1999, 69, (5), 842-856. DOI: 10.1093/ajcn/69.5.842. 8. Demay, M.B.; Pittas, A.G.; Bikle, D.D.; Diab, D.L.; Kiely, M.E.; Lazaretti-Castro, M.; Lips, P.; Mitchell, D.M.; Murad, M.H.; Powers, S.; Rao, S.D.; Scragg, R.; Tayek, J.A.; Valent, A.M.; Walsh, J.M.E.; McCartney, C.R. Vitamin D for the Prevention of Disease: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2024, 109, (8), 1907-1947. DOI: 10.1210/clinem/dgae290. 9. Are You Vitamin D Deficient? Available online: https://www.grassrootshealth.net/project/daction/ (accessed 3 December 2025). 10. McDonnell, S.L.; Baggerly, C.; French, C.B.; Baggerly, L.L.; Garland, C.F.; Gorham, E.D.; Lappe, J.M.; Heaney, R.P. Serum 25-Hydroxyvitamin D Concentrations ≥40 Ng/Ml Are Associated with >65% Lower Cancer Risk: Pooled Analysis of Randomized Trial and Prospective Cohort Study. PLoS One 2016, 11, (4), e0152441. DOI: 10.1371/journal.pone.0152441. 11. Chowdhury, R.; Kunutsor, S.; Vitezova, A.; Oliver-Williams, C.; Chowdhury, S.; Kiefte-de-Jong, J.C.; Khan, H.; Baena, C.P.; Prabhakaran, D.; Hoshen, M.B.; Feldman, B.S.; Pan, A.; Johnson, L.; Crowe, F.; Hu, F.B.; Franco, O.H. Vitamin D and Risk of Cause Specific Death: Systematic Review and Meta-Analysis of Observational Cohort and Randomised Intervention Studies. BMJ 2014, 348, g1903. DOI: 10.1136/bmj.g1903. 12. Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M.; Endocrine Society Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2011, 96, (7), 1911-1930. DOI: 10.1210/jc.2011-0385. 13. Cheng, R.Z. From Mutation to Metabolism: Root Cause Analysis of Cancer's Initiating Drivers. 2025. DOI: 10.20944/preprints202509.0903.v1; Available online: https://www.preprints.org/manuscript/202509.0903/v1. Orthomolecular MedicineOrthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org Find a DoctorTo locate an orthomolecular physician near you: http://orthomolecular.org/resources/omns/v06n09.shtml The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource. Editorial Review Board:Jennifer L. Aliano, M.S., L.Ac., C.C.N. (USA) Comments and media contact: editor@orthomolecular.org OMNS welcomes but is unable to respond to individual reader emails. Reader comments become the property of OMNS and may or may not be used for publication. Click here to see a web copy of this news release: http://orthomolecular.activehosted.com/p_v.php?c=510&m=427&s=bad97c655476f96a390a72c05a742011&d=0&v=2&l |
|
|
This news release was sent to _t.e.s.t_@example.com. If you no longer wish to receive news releases, please reply to this message with "Unsubscribe" in the subject line or simply click on the following link: unsubscribe . To update your profile settings click here . This article may be reprinted free of charge provided 1) that there is clear attribution to the Orthomolecular Medicine News Service, and 2) that both the OMNS free subscription link http://orthomolecular.org/subscribe.html and also the OMNS archive link http://orthomolecular.org/resources/omns/index.shtml are included.
|
|